《明日之子》第二季目前在腾讯视频热播当中,
李宇春的盛世美颜、吴青峰的盛世独秀、华晨宇的盛世魔音三大赛道的总共27强已经全部产生
。这些既有颜值又有才气的小哥哥将在后续的比赛当中再接再厉,为了成为真正的明日之子而努力。在《明日之子》第二季当中,不仅仅是晋级27强的选手有实力,其他的选手既然可以来到现场,也说明了他们具备自己的优势。对于他们来说,每个人都有自己对于观众的初印象。那么以下对其中有代表性的选手进行下简述,看看谁的初印象让你更喜欢。
首先还是说下
明日之子第二季27强名单
:
曾育茗、许含光、徐梦圆、蔡维泽、童儿、池一骋、孩子王、毕冉、张�豪、BB-Eight、陆政廷、文兆杰、黄翔麒、邓典、田�、段志豪、吴宇恒、郝一夫、邓泽鸣、翟潇闻、Younggee、郭震、邱虹凯、斯外戈、孙泽源、尹清、Odyssey。

盛世美颜是李宇春的赛道。晋级选手如图。

盛世美颜
李明峻
李明峻是第一个走上舞台的选手,他选择的是盛世美颜赛道,接受李宇春的考核。李明峻是一位蒙古族的选手,身高达到了180cm。李明峻的颜值让人眼前一亮,不过演唱方面有欠缺。李宇春为了鼓励后面的选手给了李明峻晋级球,但是后来被替换掉名额。

李明峻
后来曾纲杰对李明峻发起了挑战,结果两人纷纷出局,不过李明峻说:“但是你也没有晋级。”言语当中似乎透露着一些不屑,且说话的时候面露微笑。不过后台则是李明峻和曾纲杰拥抱的画面,剪辑的能力确实厉害。

李明峻说你也没有晋级
邓泽鸣
邓泽鸣说自己要把美颜赛道带领到一个新的高度,于是他向李明峻发起挑战,进行battle。邓泽鸣选择了是唱跳,演绎了一曲《绕圈》。邓泽鸣的舞台表现能力十分劲爆,颜值也上佳,于是邓泽鸣晋级成功。不过邓泽鸣的话语也是具备了攻击性,他说:“这是一个生存的游戏,不强的人就需要下来!”

邓泽鸣说不强的人就需要下来
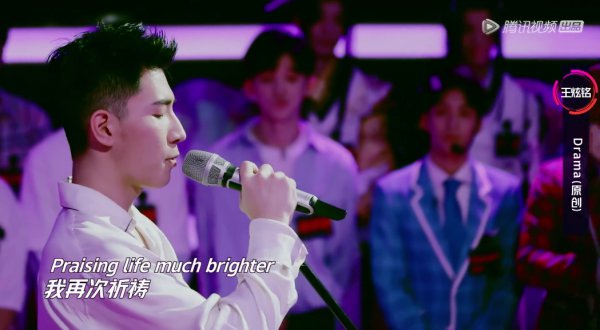
Word Wang原名王炫铭
Word Wang演唱了一首自己的原创《Drama》。且在演唱后被选中晋级。Word Wang出生于浙江温州市,从小展露对古典音乐及声乐演唱的热爱,15岁开始钢琴叙事曲的创作,并总编排音乐剧《荒诞秀》,2017年从上海戏剧学院肄业成为独立音乐人制作人同年发行首支单曲《Drama》进入演艺圈。
Word Wang演唱歌曲
陈诚
作为一位未晋级的选手,陈诚手拿一个大喇叭就来了,且向全场说要动起来,虽然陈诚没有晋级,倒是把现场的气氛变得很活跃。

陈诚
子笺子凛
这对双胞胎兄弟身着游戏服饰cos出场,演唱了一首《牵丝戏》。虽然没有晋级,但是也是独具个性的选手了。

子笺子凛
戴景耀
戴景耀的背景很好,和通过《偶像练习生》出道的蔡徐坤是好朋友。此次来参加《明日之子》第二季,戴景耀选择了一曲《宠爱》。由于是唱跳,导致现场的演唱并没有十分的流畅,遗憾的被淘汰。

戴景耀
邓一洲
个人认为,除去节目当中的一些“奇葩”类型选手,邓一洲的长相着实不够帅气。而他竟然选择了盛世美颜赛道,看来勇气十足,不过结果是被淘汰。

邓一洲
邱虹凯
邱虹凯是上届冠军毛不易推荐来的,实力可见一斑。不够邱虹凯似乎有一些紧张,手都不知道该怎么样放,但是就是由于这样的真诚和朴实,打动了李宇春。

邱虹凯
张炯敏
张炯敏上台时说:“我是炯炯”,此时一些网友很像看到何炅的表情是什么。小炯炯在演唱,而大炅炅却在后台把控全场。

张炯敏
Odyssey
这个组合可以说是第一期当中的奇葩,他们带来的海带舞,着实有些洗脑,而组合当中有一位一直戴着面具,难道你不热吗?不过就是这样的奇葩组合,征服了现场,得到了晋级球。

Odyssey
尹清
尹清可以说有十分俊俏的相貌,而他的歌声也是十分的清澈。这位一天三个时段都在变化职业的歌手一头长发,但是看上去却是十分的舒服,不像一些留着长头发的男孩那般的张狂,尹清甚至可以说是有一些女子的内秀。

尹清
一首《圆圈》通过尹清的演绎宛如天籁之声,尤其是当他在唱:“一阵风吹来,吹呀吹过来”的时候,网友的心都被迷住了,这样的嗓音,人世间也是少有的。

尹清在演唱
郭震
作为斯外戈的室友,郭震演绎了一曲王嘉尔的《巴比龙》。其实个人觉得这首歌曲郭震的唱功比起他的舞蹈功底有不足,不过这不影响郭震顺利的晋级。
郭震自信满满
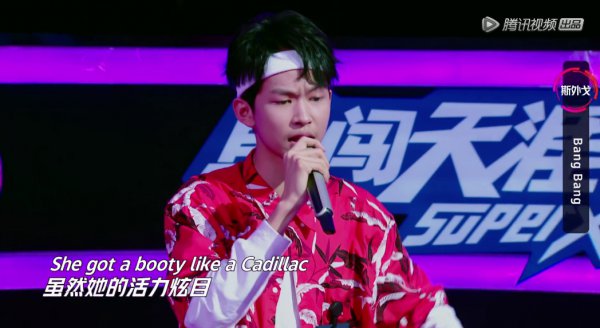
斯外戈
斯外戈是杨幂选出来的king,实力自然十足强力。斯外戈演绎了一首《BANG BANG》。整个演唱过程显得有节凑且有力,收放自如,所以斯外戈晋级是很明显的。
斯外戈
盛世独秀是吴青峰的赛道。晋级选手如图。

盛世独秀
曾育茗
曾育茗现场演绎了一场《阿通》,是他的原创歌曲。歌词写得不错,但是曾育茗却让一些网友感觉有些做作,就如他歌词当中写的一样:“我的朋友全都觉得我有一点作。”一些网友也是这样的表示。

曾育茗
晓月老板
作为很有名气的民谣歌手,晓月老板此前已经有多首代表作品,比如《探清水河》、《你好,前任》、《相思》等。晓月老板是个清秀的中年男子,或许由于年龄等方面的劣势,导致了晓月老板被淘汰。

晓月老板
李袁杰
晓月老板后出场的是国风高手李袁杰。李袁杰现场演唱了《离人愁》。这首歌曲让全场都跟着一起互动起来。但是没能打动吴青峰。不过接下来李袁杰说的话确实颇具争议。李袁杰表达了他对rapper的看法,但是却说成了popper,这让现场的rapper们很是不满,而随后李袁杰又说回了国风。前后矛盾的话语让李袁杰现场感到了压力。

李袁杰说错称呼
后来华晨宇给了李袁杰机会让他弹个和声,结果李袁杰很是懵,这也导致了三位星推官不想让李袁杰晋级了。

李袁杰不懂乐理常识
即使李袁杰的国风音乐打动他人,但是没有专业的乐理知识,就像失去地基的墙,一旦遇到压力就会出现裂缝。
徐梦圆
徐梦圆是参加选手当中唯一一个表演电音的。他现场带来的《焰火》征服了全场,也征服了星推官。

徐梦圆
赵莹
赵莹是一个就连星推官吴青峰都十分喜爱的年轻歌手。演员赵莹Cyberjelly,出生于山城重庆,毕业于四川音乐学院,自幼学习芭蕾舞数年,16岁考入四川省音乐学院流行舞专业,大一在校期间被日本艾回唱片选走,成为练习生,进行全方位的综合才艺训练,回国后签约现在的影视公司开始了新的演绎生涯。

赵莹
姜熙饶
姜熙饶显得十分的专业,她也带来了一首原创并征服了现场。中国新生代女演员姜熙饶,来自大连,身高168公,分体重46公斤,2015年因拍摄电视剧《爱情的边疆》正式进入演艺圈,2020年出演首部武侠电影《喋血群英》后又主演由香港导演颜光兴执导的电影《江湖》担任颜月一角。

余宗遥
余宗遥
这位选手虽然暂时没有获得晋级的名额,但是小哥哥的颜值还是可以的。余宗遥演唱的歌曲是一首电子摇滚乐,且这首歌曲是余宗遥自己完成的,这说明他也有写词等方面的才能,被淘汰但是不意味着他的演艺道路就此停止。

余宗遥
童儿
童儿来自一个摇滚家庭,他的爸爸也是玩摇滚的。一首《蜂巢》展示出了摇滚人的音乐态度,不妥协,不停歇。摇滚在国内的发展并不是顺风顺水,但是童儿则是个性独立。就如他的标签一样,带领和冲撞。

童儿
池一骋
池一骋是一位rapper,他的成名作品是《温州》,写的是他家乡的歌曲。这首歌曲现场演绎后星推官表示很有意思。池一骋用嘻哈的形势唱出了他对于自己故乡温州的理解,也是一位颇具个性的选手。

池一骋
杨宸哲
杨宸哲现场带来了嘻哈歌曲《忆童年》。歌曲名字就是霸气十足。不过比起他的歌曲,他的发型显然更是让大家注意,前面是类型寸头,而后面则是脏辫的设计,这样的发型也给他加了分。唱作人杨宸哲还是一个双子座的吉他老师,身高176cm,体重65kg。

孩子王
毕冉
毕冉出场,震撼全场。“合肥之子”毕冉作为king终于登场了。毕冉带来了一曲《结庐在人境》。毕冉演唱的第一句就让全场人瞬间起了起皮疙瘩,接下来就是毕冉的说唱表演时间。这首歌曲把现场带入到了毕冉的世界当中,避开所有的世间纷扰,只想找到属于自己的世外桃源。

毕冉
毕冉的歌声极具引力,同时毕冉的颜值也是不错。眉毛浓厚,面貌给人亲近感。和其他的rapper不同,毕冉没有什么“奇异”的发型或者是“刻意”的服饰,毕冉只想做自己,把自己的毕冉style展示出来。就连杨幂也比心给毕冉,毕冉则是时刻保持着自己的态度。

毕冉在演唱
张�豪
张�豪参加过第一季的《明日之子》。此次再来,自然是有备而来。张�豪演唱了一曲《肆无忌惮》。这是一首原创歌曲,由薛之谦作词。歌词满满都是薛氏风格,而张�豪的演绎也是打动人心。不过歌曲带有薛氏情歌的风格,张�豪还是要继续加油。

张�豪
张�目
这是《明日之子》第二季当中最难写的名字了,这个字念“hù”。是美好的意思。张�目年纪很小,看上去也是稚气未脱,即使扎起了马尾,弹起了吉他,但是满脸的孩子气。最终张�目遗憾被淘汰。

张�目
4盛世魔音 你的好声音在这里将主宰一切
盛世魔音是华晨宇的赛道。晋级选手如图。

盛世魔音
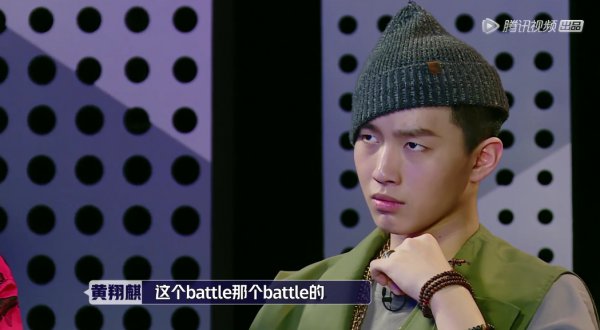
黄翔麒
在看到舞台上很多不是rapper 的选手说要互相battle的时候,黄翔麒有些不开心,因为battle是嘻哈的术语,但是他们真正的rapper都没有说话,其他人似乎没有资格。
黄翔麒不满
黄翔麒现场演绎了一曲《RAP GOD REMAKE》,歌词霸气,黄翔麒的演绎也是恰到好处,黄翔麒用自己的实力证明了杨幂选择他成为king是正确的。
黄翔麒在rap
文兆杰
文兆杰的一曲原创《呼吸》,让现场进入到了一个属于文兆杰的世界当中,这首歌曲歌词有深度,而文兆杰的嗓音十分的特别,给人一种无法抗拒的吸引力。此时华晨宇再次忍不住要抢人了。而吴青峰甚至说你想要什么词我都写给你。足以见得文兆杰的歌曲是多么的余音绕梁。

文兆杰
BB-Eight
这位rapper的口气很大,但是个人觉得作品并不是等同他的话语。这位选手出来的时候大家都在弹幕说像《创造101》的Yamy,不过看到这张照片个人觉得眼睛又有一些像王俊凯。

BB-Eight
席旭泽
1990年出生于山西大同的席旭泽的淘汰确实很可惜。他现场带来了一曲《伊人》。这首歌此前在《偶像练习生》当中钱正昊也是有所演绎。当时钱正昊演绎的时候被誉为天籁再现。现在席旭泽也带来了他自己的版本。席旭泽版本的《伊人》显得更加成熟,并能打动其他人。

席旭泽
备注:
山东省互联网传媒集团主办 Email:
webmaster@dzwww.com
新闻信息服务许可证
音像制品出版许可证
鲁ICP备09023866号
新出网证(鲁)字02号
网络视听许可证
违法不良信息举报电话:0531-85196540